

Adherence was assessed using PDC and the proportion of adherent patients, who were defined as patients with PDC ≥0.8 and, as a sensitivity analysis, PDC ≥0.5. Study outcomes evaluated during follow-up included adherence and persistence to triple therapy, as well as descriptive treatment patterns of the FF/UMEC/VI and the MITT cohorts. Patients with an asthma diagnosis during baseline were not excluded but were accounted for in the adjustment method. Patients were excluded if they used MITT during the baseline period. Diagnosis of COPD was identified with International Classification of Disease, 10th revision, Clinical Modification codes J41.x–J44.x. In addition, patients were required to have at least two diagnoses of COPD in an outpatient setting, or at least one diagnosis of COPD in a hospitalisation or emergency department (ED) setting, during the baseline period or on the index date.

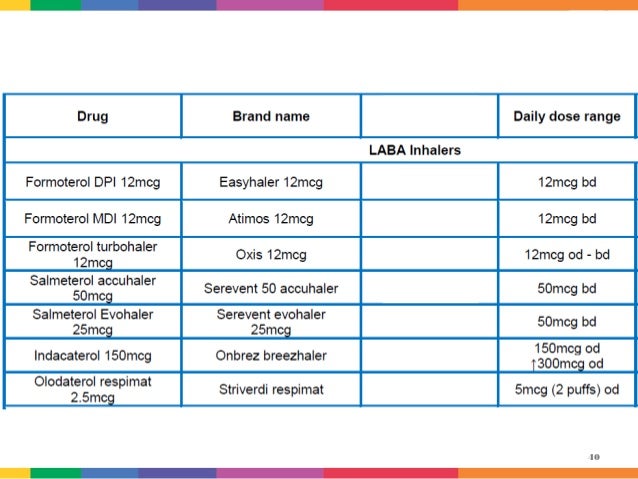
Patients aged 40 years or older at index were required to have at least 12 months of continuous health insurance coverage prior to the index date and at least 6 months of coverage following the index date. Patients had at least one dispensing of single-inhaler FF/UMEC/VI (100/62.5/25 mcg) or, if none, at least one overlapping day of supply with all three components of triple therapy (i.e., ICS, LAMA, and LABA) on or after 18 September 2017 (as a sensitivity analysis, MITT was also identified using a 30-day overlap of supply). Persistence and treatment patterns were evaluated post-index up to 12 months of follow-up. Adherence to triple therapy was evaluated at 6 months of follow-up and, separately, among the subgroup of patients with at least 12 months of follow-up. The follow-up period, which was at least 6 months long, spanned from the index date to health plan disenrolment or end of data availability, whichever occurred first. The baseline period was defined as the 12 months before the index date. For MITT users, the index date was the first overlapping day of supply with all three components of triple therapy (ICS, LAMA, and LABA), which could be via three separate inhalers (ICS + LAMA + LABA) or two inhalers (ICS/LABA + LAMA or LAMA/LABA + ICS) patients receiving ICS/LABA + LAMA/LABA were not included in the study population. The index date was defined as the date of triple therapy initiation. LABA are also long-term control medicines.This was a retrospective weighted cohort study of patients with COPD initiating triple therapy between 18 September 2017 (FDA approval date for FF/UMEC/VI) and 30 June 2019. Bronchodilator medicine opens the airways in the lungs by relaxing smooth muscle around the airways. Long-acting beta-agonist ( LABA) are a type of bronchodilator medicine. It antagonises the effect of acetylcholine, which is the main neurotransmitter in the parasympathetic nervous system of the airways. Tiotropium bromide is a long-acting muscarinic antagonist ( LAMA). LAMAs include: Incruse ® (umeclidinium), Take once daily using Ellipta ®.Īlso, what is a lama in COPD? Global initiative for COPD suggests the use of long acting beta agonists (LABA) and long acting muscarinic antagonists ( LAMA) in combination for group B patients with persistent symptoms, group C patients with further exacerbations on LAMA treatment and for group D patients with or without the addition of inhaled LABA and LAMA are types of bronchodilators. Long-acting bronchodilators can be either LABAs (long-acting beta2 agonists) or LAMAs (long-acting muscarinic antogonists). Long-Acting Bronchodilators These medications are long-acting. Long-acting bronchodilators such as long-acting β-agonist (LABA), long-acting muscarinic antagonist ( LAMA), and LABA/inhaled corticosteroid (ICS) combinations have been used in people with moderate to severe chronic obstructive pulmonary disease (COPD) to control symptoms such as dyspnoea and cough, and preventĪlso to know is, what is a lama medication?


 0 kommentar(er)
0 kommentar(er)
